 Martin Kudr, MD, PhD
Martin Kudr, MD, PhD
is a physician-epileptologist and head of the paediatric epilepsy surgery programme at the Department of Paediatric Neurology at the Second Faculty of Medicine, Charles University, and Motol University Hospital. His main research interests include clinical science in the field of epileptology and epilepsy surgery, especially functional imaging, SEEG, and insular epilepsy.
 Matyáš Ebel, MD, BSc
Matyáš Ebel, MD, BSc
is a secondary physician and doctoral student at the Department of Paediatric Neurology at the Second Faculty of Medicine, Charles University, and Motol University Hospital. He studied General Medicine at the Second Faculty of Medicine, Charles University, and Cybernetics and Robotics at the Czech Technical University. He specialises in epilepsy surgery with an emphasis on the analysis of intracranial EEG (iEEG), high-density EEG (HD-EEG), and neuroimaging, especially in patients with tuberous sclerosis.
The paediatric epilepsy surgery programme has been led by Prof. Pavel Kršek at the Department of Paediatric Neurology at the Second Faculty of Medicine, Charles University, and Motol University Hospital for 25 years. It provides care for children with epilepsy from the Czech Republic, Slovakia, and other European countries. In 2024, the 500th patient was operated on, and the success rate of eliminating seizures increased to 80 percent. The Epileptology Research Centre (EpiReC) is involved in the implementation of innovative diagnostic and therapeutic procedures.
How do epilepsy foci form in the brain?
Martin Kudr: Most often due to congenital malformations of cortical development, benign tumours, less commonly due to brain damage around the time of birth, or, for example, in tuberous sclerosis. The epileptogenic zone, where brain cells are activated more than they should be, is usually one. However, in some severe patients, typically with focal cortical dysplasia type 1, it can be scattered over a larger part of the brain.
Matyáš Ebel: Patients with tuberous sclerosis can also have multiple seizure-generating foci. However, usually, only one place, the hub of the network, is the most active, and that is what we try to locate and surgically disrupt.
If you remove the affected cells, what happens to the resulting space? One of your patients had about a quarter of her brain removed this way.
M. K.: It fills with cerebrospinal fluid, which normally cushions impacts throughout the brain, and scarring forms at the edge of the resection. This does not limit the patient in the long term; within two months after surgery, they can play football, for example. The scar is just a cosmetic defect; there may be an unevenness or a groove in the bone underneath. Paradoxically, cognitive performance usually improves after removing part of the brain because seizures no longer harm the brain.
Do epileptogenic zones correspond to functional brain centres? For example, does epilepsy of the motor centre manifest in the limbs?
M. E.: It can be. The areas of the brain where seizures begin can be close to so-called eloquent areas, which are responsible for higher functions – movement, speech, attention, or memory – or sometimes they can even overlap. If a patient has cortical dysplasia near the motor centre for a limb, seizures can manifest as jerking of that limb. When planning surgery, it is crucial to determine exactly where the motor pathways run, prepare imaging data for the surgeon, and then proceed as gently as possible, with motor monitoring.
Why is it so important to respond and treat early, especially in the youngest infants?
M. K.: The developing brain is more susceptible to damage from severe epilepsy. If we respond early, we give the brain a chance to minimise damage, and the child can develop as normally as possible. In epileptology, the paradigm is currently changing worldwide. We do not wait to see if epilepsy progresses to a very severe form – if we see an opportunity, we operate on the child earlier, often already in infancy.
What examinations must a patient undergo to learn about all the significant zones and pathways?
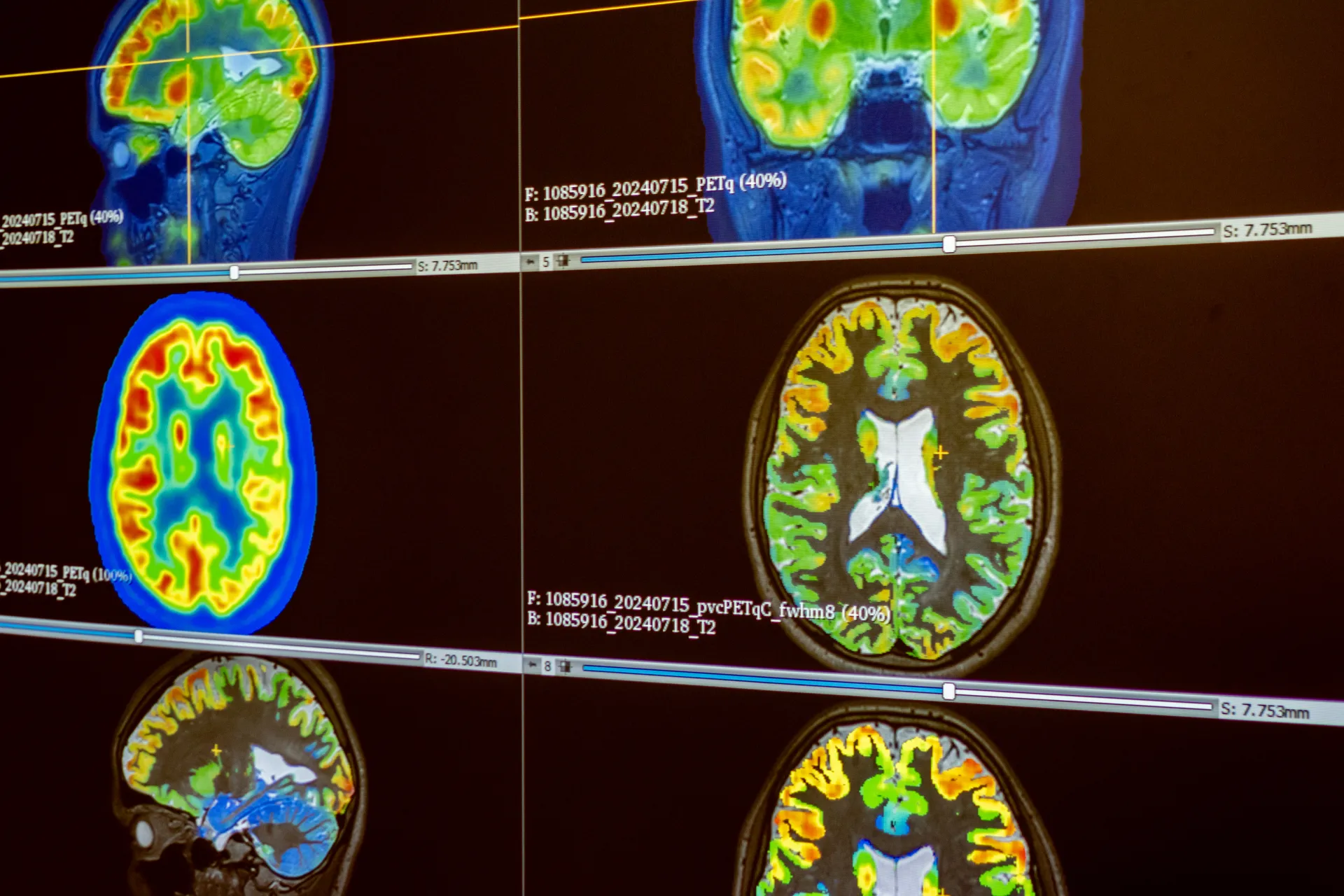
M. E.: The first in the basic range of examinations is video-EEG. This determines brain activity outside of seizures and ideally during a seizure, while we also record the patient on video and evaluate the course of the seizure. Next is magnetic resonance imaging, FDG-PET modified by the pvc-PET method, and neuropsychological examination. If necessary, we supplement with other functional neuroimaging or electrophysiological examinations.
Let's stop at pvc-PET, because engineers from the Czech Technical University played a significant role in its development. The team led by Radek Janča improved the older FDG-PET imaging to better map the metabolic activity of tumour cells. How does it work?
M. K.: Pvc-PET significantly improves FDG-PET itself. The principle is that in the brain area where less sugar is consumed, there is usually also an epileptogenic zone. PET shows this, but the images are coarse and difficult to navigate. One improvement is that PET images are fused with magnetic resonance imaging, which significantly refines the localisation of the epileptogenic zone.
M. E.: To this the limiting condition is added is that the brain's metabolism is mainly generated by the cerebral cortex. This removes the PET signal from the white matter, further refining the examination. Such images are also easier to view.